Antivenoms for the World:
Building an Asia–Pacific Snake Antivenom Network
Cindy Li / photos courtesy of Taiwan CDC / tr. by Phil Newell
July 2024

The study of snake venoms is a branch of science that has thrived in Taiwan. (photo by Kent Chuang)
Looking back over the past 100 years, the efforts of many scientists, including Tu Tsung-ming, Lee Chen-yuan, and Chang Chuan-chiung, put Taiwan on the global map in the field of snake venom research. Today, the strong foundations that they laid down are being built upon by their successors, who are poised to do their part to help the 2 million people worldwide who suffer snakebites each year.
Statistics from the Taiwan Centers for Disease Control (Taiwan CDC) indicate that each year about 1,000 people in Taiwan are bitten by poisonous snakes. The main culprits are six major venomous snake species: the Chinese green tree viper (Trimeresurus stejnegeri), the Taiwan habu (Protobothrops mucrosquamatus), the many-banded krait (Bungarus multicinctus), the Chinese cobra (Naja atra, a.k.a. the Taiwan cobra), the hundred-pacer (Deinagkistrodon acutus), and Russell’s viper (Daboia siamensis). Anyone who is bitten can head to any healthcare facility nationwide and get an injection of antivenom to neutralize the snake venom and minimize symptoms of toxicity.

Unlike the clear images found in field guides, photos of snakes that medical personnel are shown in emergency rooms are often dark and blurred. (photo by Kent Chuang)
Help for emergency-room doctors
The first basis doctors use for diagnosing snakebites is a description of the snake, but in fact there is considerable difficulty in identifying the snake involved in each case. For example, Russell’s viper, the hundred-pacer, and the Taiwan habu all have similar bold patterns on their bodies, with the differences between them being in the details.
Cheng Kai-wen, a doctor in the Department of Occupational Medicine and Clinical Toxicology at Taipei Veterans General Hospital (TVGH), points out that all emergency-room doctors in Taiwan are knowledgeable about the six major venomous snakes, and so are able to handle most cases of snakebite. However, if the identification of the snake species involved is in doubt, or if atypical symptoms appear in the course of the patient’s treatment, the attending doctors will call the Taiwan Poison Control Center (TPCC) at TVGH.
Emily Chen (Chen Hsiang-ling), a pharmacist at the TPCC, relates that thanks to vigorous public awareness campaigns by the government and the widespread use of smartphones, in recent years there has been an increase in the number of victims taking photos of the snakes that bit them. “However, people are often bitten late at night or in the evening, so the quality of the photos tends to be less than ideal.”
By way of example, Cheng Kai-wen cites a recent case in which someone was bitten by an Alishan habu. The hurried photo that the victim took was dark and incomplete, making it quite different from the clear, complete images of snakes found in traditional illustrated field guides. For the doctors at the TPCC, who have for many years been assisting other doctors in identifying snake species, this kind of problem is very challenging.
To deal with this issue, at the suggestion of Chen Kuang-ting, a doctor from Changhua’s Show Chwan Memorial Hospital who was seconded to the TPCC team only last year, Cheng Kai-wen and Emily Chen contacted Lin Te-en, an associate researcher at the Taiwan Biodiversity Research Institute and founder of the Taiwan Roadkill Observation Network, to ask about the possibility of compiling a training database for identifying those species of terrestrial snakes whose victims often end up in emergency rooms.
After several months of optimization, the database went online in January of 2024. Using their mobile phones, doctors can practice identifying the carcasses of multiple snake species, like playing a game. At the same time they can learn relevant information such as the regional distribution of each species and their salient characteristics, thereby rapidly improving their skill at identifying these creatures.
Chen Kuang-ting demonstrates how the database is used by analyzing a photo of a snake carcass of which only the rear part remains. He tells us that although it has no head, by looking at the characteristics of its midsection and tail, it can be identified as a Chinese cobra. He further explains that these cobras are usually gray, black, or brown in color, and one cannot distinguish their iconic markings unless their hoods are opened out. Thus, he says, “To some extent the database accurately reflects the characteristics of snake carcasses or photos that people may bring to the emergency room.”
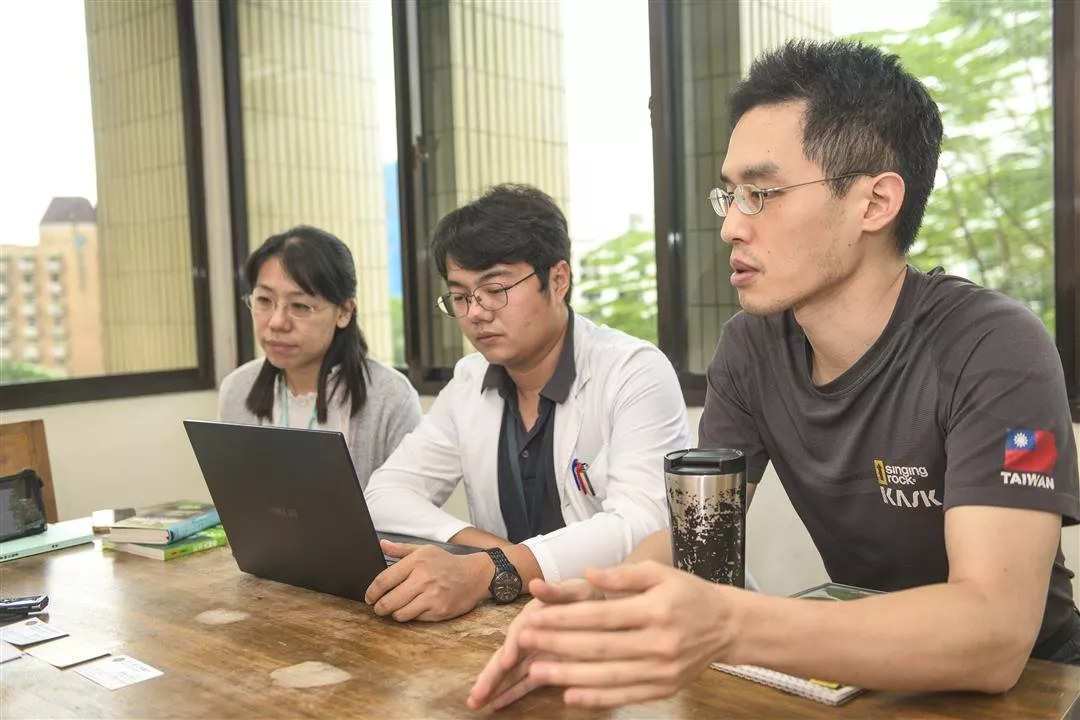
At the suggestion of Dr. Chen Kuang-ting (center) of the Taiwan Poison Control Center at Taipei Veterans General Hospital, his colleagues Dr. Cheng Kai-wen (right) and pharmacist Emily Chen (left) worked with the Taiwan Biodiversity Research Institute to create a database to train doctors in identifying the venomous snakes that frequently cause snakebite injuries. (photo by Kent Chuang)
The difficulties of snake identification
If a doctor has no information at all about the species of snake that bit an incoming patient, the next clue for diagnosis is the clinical symptoms. However, the complexity of assessing clinical symptoms is compounded by the different amounts of venom that may have been injected, the physical constitution of the patient, and the possibility of a dry bite (a bite that injects no venom into the wound), or that the snake that made the bite was non-poisonous.
Hung Dong-zong, a doctor in the Poison and Toxicology Counseling and Testing Center at China Medical University Hospital, notes that among the six major venomous snake species, one example of a diagnostic challenge is the difficulty of distinguishing between the bites of the Taiwan habu and the Chinese cobra.
Most patients in Taiwan reach an emergency room within an hour of being bitten, but in the majority of cases there are no obvious changes in the wounds during this time. Moreover, the black-blue discoloration caused by ulceration around the bite wound from a Chinese cobra, and the bruising from the bite of a Taiwan habu, are difficult to immediately differentiate even for experienced medical personnel.
If the doctor decides to inject the patient with the antivenom for the Taiwan habu (which is also used for bites of the Chinese green tree viper), but after several hours of observation the patient shows no clear improvement and the wound begins to show ulceration and necrosis (tissue death), it is only then that the doctor can be certain that the patient was attacked by a Chinese cobra. At that point the physician must inject the patient with the corresponding antivenom, with the whole process requiring about six hours of observation.
For every second that a doctor waits, the chances of complications may increase. Studies show that about 50% of cobra venom consists of cytotoxins (poisons that damage cells). Hung Dong-zong notes that if an antivenom is not given quickly, these cytotoxins will cause necrosis and increasing ulceration. Even after the toxins are neutralized, the patient is likely to need multiple follow-up surgeries to remove dead, injured and infected tissue. In serious cases the affected body part may have to be amputated, leaving the patient with a lifetime deformity.
Speaking of the need to quickly identify the snake species involved in snakebite cases, Hung pointed out in his 2002 doctoral thesis: “If acting only on the basis of clinical symptoms, it is often impossible to make an accurate determination and administer the correct antivenom. There is a need for more objective assessment methods for use in clinical settings.”
Ultimately, Hung himself successfully developed a powerful tool to address this need.

Chinese cobra
Goose eggs to the rescue
In 2008, Hung developed Taiwan’s first rapid screening test for cobra venom, which is called the immunochromatographic test of cobra venom, or ICT-Cobra. After a patient’s blood is drawn, a centrifuge is used to separate out the serum, which is dripped onto a test cassette and produces a final result within 20 minutes after taking the blood sample.
The key to success was a goose egg.
Internationally, rapid test kits for snake venom have also been developed in India and Myanmar. “There have to be two kinds of antibodies in the test cassette. One is from horses, which produce the kind of antibody that is currently used in antivenom. For the other, some people use antibodies from rabbits, others from mice. The problem lies in choosing which animal to use as the antibody source other than the horse.” Hung goes on to explain: “When we first started, nothing we did worked, until one day we used goose eggs and discovered that their antibodies were beautiful.” This outcome prompted Hung to work with the Changhua Animal Propagation Station to inject treated snake venom into geese, gather the eggs laid, and extract yolk immunoglobulin (IgY) to use in experiments with rapid test cassettes.
The results were exciting for Hung and his team. The ICT-Cobra test not only accurately identifies cobra venom, it can detect it at levels as low as five nanograms per milliliter (5 ng/ml). He says with a smile that a large part of the credit for this outcome is due to Taiwan’s high-quality goose farming industry.
In addition, this rapid test for cobra venom, which costs only NT$300 per cassette to make, has been exported from Taiwan, becoming an important item in an ongoing program to build a Taiwan–Vietnam Anti-Venom Network.

Photos of snake carcasses submitted by the public to the Taiwan Roadkill Observation Network have become tools for emergency-room doctors to learn to identify snake species.(photo by Kent Chuang)
An Asia–Pacific antivenom network
When it comes to friendly collaboration between Taiwan and Vietnam in the field of healthcare, in addition to the excellent foundation laid down by nearly ten years of work in Vietnam by Taipei Medical University, there has also been cooperation in other areas. Sung Wang-chou, associate researcher in the National Institute of Infectious Diseases and Vaccinology (NIIDV) at the National Health Research Institutes (NHRI), notes that another event that became a bridge for friendship between the NHRI and Children’s Hospital No. 1 in Ho Chi Minh City was an outbreak of enterovirus in Vietnam in 2011. At that time, a laboratory for infectious disease research that the NHRI, under the leadership of former NIIDV director Su Ih-jen, had founded in 2006 in collaboration with Children’s Hospital No. 1, provided assistance in conducting molecular epidemiology research and establishing a screening process to make it possible to rapidly bring the outbreak under control.
In recent years, through its interactions with Children’s Hospital No. 1, the NHRI has learned that Vietnam has difficulties in treating snakebite in children. “Children’s bodies are smaller than adults’ bodies, so the toxins act much faster,” says Sung. This makes it all the more important to rapidly identify the snake species involved.
Fortunately, experiments with the ICT-Cobra test, which was developed to identify the venom of the Chinese cobra (Naja atra), have shown that it is also effective in identifying the venom of the Indochinese spitting cobra (Naja siamensis), the monocled cobra (Naja kaouthia), and the Indian cobra (Naja naja). For these three species, the test’s sensitivity ranges from five to 50 ng/ml. This represents an opportunity for Taiwanese rapid venom screening technology to make an entrée into Southeast Asia.
Statistics from Cho Ray Hospital in Ho Chi Minh City indicate that in 2016 that hospital alone received more than 1,000 snakebite cases. These mainly involved the white-lipped pit viper (Trimeresurus albolabris), with at least 660 cases, and the Malayan pit viper (Calloselasma rhodostoma) with at least 154.
In response to this situation, in 2022 a program was launched under Taiwan’s New Southbound Policy to construct an Asia–Pacific antivenom research network, in order to facilitate the application of rapid testing to the Malayan pit viper.
Sung Wang-chou shares with us that at present, successful testing for venom of the Malayan pit viper requires a minimum concentration of 50 ng/ml. However, he says, “This is an adequate level of sensitivity.” He further reveals that an NHRI team is currently working with Hung Dong-zong and Vietnam’s Institute of Vaccines and Medical Biologicals (which produces antivenoms and numerous vaccines) to develop a rapid test kit that can simultaneously screen for the venoms of Russell’s viper, the Chinese cobra, and the Malayan pit viper. “The validity of the test results is very high.”

Patients bitten by the Chinese cobra and the Taiwan habu initially show similar symptoms. Even experienced medical personnel cannot easily distinguish between them.
Taiwan can help
Besides developing rapid screening tests for snake venoms, the program is also working on the use of recombinant snake venom proteins to produce broad-spectrum antivenoms.” This involves using bioengineering to produce antivenoms in the laboratory, breaking free of the limitations imposed by the regional nature of snake venom collection. Thus antivenoms for Southeast-Asian snake species can be produced in Taiwan. Sung says: “They are more cost-effective than horse antivenoms, and can eliminate the costs of keeping snakes as well as the risk of workers being injured while collecting venom.” One day this breakthrough technology may be able to help save lives around the world.
The World Health Organization (WHO) states that the regions where venomous snakebite injuries are most common are Africa, Asia, and South America, and that injecting antivenoms is the most effective treatment.
However, statistics show that the annual supply of 280,000 doses of antivenom for all of Southeast Asia falls far short of what is needed for the 240,000 cases of snakebite in the region each year. Correct use of antivenoms not only can save lives, it can prevent economic losses estimated at US$6,400 per patient and a reduction of nearly 0.1 percentage points in annual GDP growth in the region.
Accordingly, in 2017 the WHO listed venomous snakebite as one of the world’s high-priority neglected tropical diseases. It hoped that more resources could be committed to developing novel antivenoms and rapid test kits to achieve the goal of reducing deaths and disability from snakebites by 50% by 2030.
Sung Wang-chou states that when the NHRI’s Bioproduction Plant 2 is completed, this will greatly increase domestic production capacity for antivenoms. If this is accompanied by a strategy of using recombinant snake venom proteins to develop and manufacture antivenoms to meet the needs of different regions, this not only can strengthen Taiwan’s collaborative relationships with other countries in the field of public health, but may also provide an entrée to international markets. “Antivenoms from Taiwan may very well find a whole new future,” he predicts.

Snake venom immunogen is injected into horses, and once the animals produce sufficient antibodies, these are extracted from their blood serum and used to make antivenom.

The venomous snake laboratory at the Taiwan CDC has installed snake enclosures to hold the six major species of venomous snakes found in Taiwan. The goal is to ensure a reliable supply of snake toxins for domestic production of antivenoms.

Sung Wang-chou, associate researcher in the National Institute of Infectious Diseases and Vaccinology, and his team often travel between Taiwan and Vietnam as they work to build an Asia–Pacific antivenom research network. (photo by Jimmy Lin)

In May, 2024 Taiwan’s National Health Research Institutes signed a contract with Children’s Hospital No. 1 in Ho Chi Minh City, Vietnam, to conduct research using clinical samples from child snakebite patients. The photo shows NHRI vice president Wei J. Chen (second from left) with Dr. Nguyen Thanh Hung (second from right), director of Children’s Hospital No. 1. (courtesy of Sung Wang-chou)

A delegation of academics led by Nguyen The Dung (fifth from left), former director of the Ho Chi Minh City Department of Health, visited the National Institute of Infectious Diseases and Vaccinology to learn about Taiwan’s production process for antivenoms. (courtesy of Sung Wang-chou)

The only solution to venomous snakebites is a reliable supply of high-quality antivenoms. Contributing to this supply is one way in which Taiwan can help protect lives all over the world. (photo by Jimmy Lin)
@List.jpg?w=522&h=410&mode=crop&format=webp&quality=80)

@List.jpg?w=522&h=410&mode=crop&format=webp&quality=80)
@List.jpg?w=522&h=410&mode=crop&format=webp&quality=80)

@List.jpg?w=522&h=410&mode=crop&format=webp&quality=80)
@List.jpg?w=522&h=410&mode=crop&format=webp&quality=80)
